Nursing Interventions You Need to Know to Promote Adequate Respiratory Function
Introduction
Aim
Definition of Terms
Cess
Direction
Special Considerations
Evidence Table
References
Introduction
Children who experience respiratory distress may benefit from avant-garde secretion clearance techniques to optimize oxygenation and ventilation. Physiotherapists as well provide this service within the hospital, but are not available during all hours. Should it exist identified that physiotherapy input is required for secretion clearance, then a physiotherapy EMR referral should be completed, and physiotherapy contacted if within hours. This guideline should be utilised to guide advanced secretion clearance outside of physiotherapy hours, where a physiotherapy treatment programme does not yet exist, or if a plan has been pre-discussed with nursing staff. Airway suctioning volition not exist discussed in this guideline every bit this is covered in local guidelines depending on department vigil.
Aim
- Outline of appropriate patient groups for advanced secretion clearance
- Outline the role of nurses in different departments for advanced secretion clearance techniques
Definition of Terms
- ARDS: Acute Respiratory Distress Syndrome
- ETT: Endotracheal tube, and artificial airway bypassing the vocal cords to provide airway and ventilation back up
- Transmission hyperinflation: A bagging technique performed in ventilated patients which utilises a tedious inspiration (to approx. twenty% greater than set PIP), followed past an inspiratory hold and rapid exhalation
- Mechanical In-exsufflation: Use of a mechanical device (e.chiliad. CoughAssist®) to provide cycles of insufflation and exsufflation pressures to the lungs to facilitate secretions clearance
- PEP: Positive expiratory pressure techniques (eastward.g. PEP mask, chimera PEP) are prescribed by physiotherapists to facilitate secretion clearance by providing an expiratory resistance which can improve collateral ventilation, inflation of partially airtight lung units and secretions clearance.
- PICU: Paediatric Intensive Care Unit
- PIP: Peak Inspiratory Pressure
- SMI: Performance of a voluntary Sustained Maximal Aggrandizement at the meridian of a deep inspiratory jiff whereby the breath is held for 2-iii seconds before exhalation. Used to facilitate recruitment of poorly filled lung units.
Assessment
Criteria for advanced secretion clearance:
1. Advanced secretion clearance should non be considered routine and the rationale for treatment should exist based on excessive secretions, atelectasis or abnormal gas exchange.
2. Collaboration with physiotherapists regarding the patient'due south cardiorespiratory physiology, chest mechanics and evidence for these techniques is essential.
Patient assessment should include:
- Nursing cess: See Nursing cess
- History: Antenatal and birth history, weight, co-morbidities, medications
- Respiratory assessment: See assessment of severity of respiratory conditions
- Auscultation: Mind for evidence of secretions or decreased air entry
- Review of contempo chest 10-ray: Testify of consolidation or lobular plummet, 'ground glass' appearance equally seen in ARDS
- Review patients' level of tolerance for handling and fatigue level- consider recent sleeping patterns. Over treatment can be as harmful equally undertreatment.
- Review recent laboratory results: Blood gas, FBE, platelets
- Assessment of patients' hurting level using appropriate hurting tool
Advanced secretion clearance techniques tin contribute to haemodynamic instability, further respiratory compromise and rib fractures if performed inappropriately. Therefore careful assessment should be undertaken to appraise if the intervention is likely to be of benefit and whether there are any contraindications to treatment.
Table 1 outlines which weather condition have been acknowledged every bit receiving benefit from advanced airway clearance techniques strategies by a nurse. Other weather condition which are deemed as having no do good from avant-garde airway clearance should not be undertaken unless past a physiotherapist.
Related Clinical Practice guidelines
- Tracheostomy management
- Artificial airway suctioning *intranet only
- Continuous Positive Airway Pressure (CPAP) and Non-invasive Ventilation (NIV)
- Non-invasive respiratory support in PICU guideline *intranet just
- Nursing management of the patient with invasive mechanical ventilation in PICU *intranet simply
Table 1:
| Patient condition | Strategies initiated past nurse |
| Chronic disease with large amounts of sputum
| Encourage patient to complete usual (home) airway clearance technique Positioning Chest percussion and vibrations Manual hyperinflation (intubated) * PICU but Deep breathing with SMI and coughing Review from physiotherapist |
| Acute lobar atelectasis (ventilated) | Adequate ventilation, bagging, manual hyperinflation * PICU only Review from physiotherapist |
| Atelectasis (mail service extubation) | Deep animate with SMI and cough Positioning and mobilisation Encourage patient to consummate usual home airway clearance regime if applicable |
| Pneumonia in a neurologically compromised child (due east.g. Cerebral Palsy) | Positioning and sitting out of bed. Manual hyperinflation (intubated) *PICU merely Review from physiotherapist |
| Pneumonia in a typically developing kid/Pneumonia in kid with no other co-morbidity (ventilated) | Manual hyperinflation *PICU only Review from physiotherapist if ongoing sputum memory issues or unable to clear secretions with nursing strategies alone. |
| Neuromuscular illness | Review from physiotherapist |
| Intubated neonate | Review from physiotherapist |
| Trauma | Deep breathing with SMI and cough Positioning and mobilisation within scope of injury. Review from physiotherapist if ongoing sputum retention problems |
Table ii
| Conditions where respiratory physiotherapy is NOT indicated | Pneumonia in typically developing child/ with no comorbidity (not-ventilated) Bronchiolitis Acute asthma/severe bronchospasm Croup ARDS |
Management
Nursing scope of practice will vary in regards to the caste of advanced secretion clearance that tin be provided in unlike departments in the infirmary. Non-intensive care areas are differentiated from the PICU due to variations in scope of practise and the clinical environment.
Please consider patients illness profile when selecting treatment options, and ever seek guidance from medical colleagues when planning to provide avant-garde secretion clearance.
Tabular array 3
| Advanced secretion clearance treatment technique | Contraindications (exercise Not perform technique) | Precautions (seek medical clearance prior) |
| Percussions and vibrations |
|
|
| Positioning and sitting out of bed |
|
|
| Deep breathing with SMI and cough |
| |
| Transmission hyperinflation (PICU only) |
|
|
| Bubble PEP** |
|
|
Non intensive intendance areas
Effective cough:
- Appraise if developmentally appropriate and patient tin follow instructions
- Position patient in an upright position supporting their caput and neck if require
- Provide adequate analgesia and support of any surgical wounds or sutures to prevent damage. For instance holding a pillow or folded towel in forepart of their chest for sternal wound
- Enquire patient to take a few deep breaths and detect the expansion of their thorax
- Ask the patient to take a deep breath and hold information technology at the pinnacle of inspiration
- Ask the patient to "huff" a few times then followed by a hard "huff" at the end of inspiration- this should trigger a coughing
Postural drainage positions:
- Postural drainage utilises the patient position to facilitate the removal of secretions with gravity. In children modified postural drainage positions are used that do not involve any head-downwardly positions
- Auscultate the chest to determine the areas of the breast that demand drainage
- Administer appropriate pain relief and explain the procedure to the patient
- Bronchodilators, nebulised saline or mucolytic agents may exist administered prior to repositioning if prescribed
- Position the patient with the affected lung segment positioned uppermost, utilize pillows to maintain patient's position. If this does not announced to be having do good or the patient is desaturating in this position effort lying on the other side as some patients will clear more than secretions from the dependent lung.
- Encourage patient to cough or suction the patient's airway to aid in secretion clearance.
- Monitor the patients HR, RR and Sp02. Discontinue postural drainage (or change the postural drainage position) if tachycardia, dyspnoea or hypoxia occur.
Mechanical in-exsufflation (due east.yard. CoughAssist®):
- Mechanical in-exsufflation should only be performed in patients who take already been commenced on the handling by a physiotherapist.
- Nursing staff should merely perform mechanical in-exsufflation if they take attended an almanac education session by a physiotherapist or have had bedside grooming with a physiotherapist in the past year. A patient-specific review and handover by a physiotherapist is also advised.
- Position the patient accordingly ensuring their caput is supported.
- Check the settings on the mechanical in-exsufflation device against those prescribed for the patient in the EMR order
- Provide a mechanical in-exsufflation bicycle every bit outlined in the EMR social club, clear secretions via suction and repeat equally needed (monitoring for fatigue)
- Setting prescriptions should merely be modified by a physiotherapist.
Rosella (PICU)
Effective coughing:
- When extubated, follow instructions every bit above
Postural drainage positions:
- Equally above
Mechanical in-exsufflation (due east.yard. CoughAssist®):
- As above
Deep animate with SMI post-obit extubation:
- Provide adequate pain relief
- Maintain the patients head in an neutral position with the bed elevated 30 to 40 degrees
- Educate the patient to take a deep jiff and hold it for approximately 3 seconds, encourage them to do this at least 10 times every hr
- Include the parents in the didactics and encourage them to prompt their child each hour
- Provide a rolled upwardly towel or pillow to patients who have undergone a sternotomy or other surgery to the thorax or abdomen and encourage them to hug the towel to their chest or wound site when coughing to minimise discomfort
Chest percussion and vibrations:
- Vibrations and percussions may exist used in chronic illness with large amounts of sputum due east.g. Cystic Fibrosis
- Obtain a physiotherapy assessment in all patient groups prior to using this technique
- Position the patient according to location of specific lung pathology (or perform in alternate side-lie)
- Ensure adequate padding with employ of a folded towel over the rib area
Percussion:
- Place patient in optimal postural drainage position
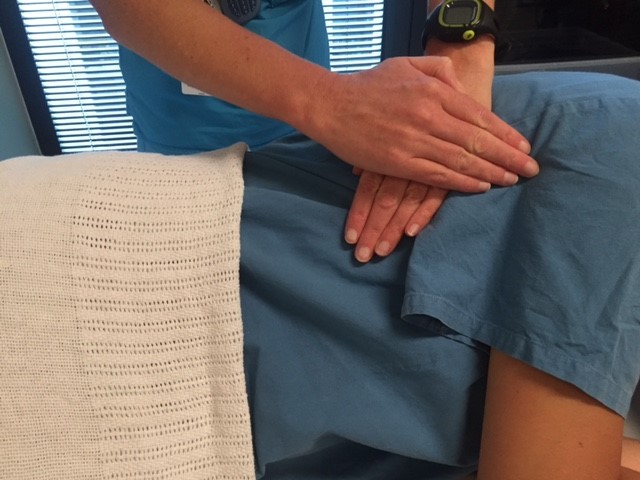
- Perform rhythmic, firm tapping to the chest wall using a cupped paw over a segment of lung that has demonstrated consolidation or collapse (run across figure 1)
- Never perform on bare skin or over surgical incisions, beneath the ribs or over the spine or breasts due to risk of tissue damage
- Percuss area for up to 5 minutes
Figure 1: Hand position for chest percussions

Vibration:
- Place patient in optimal postural drainage position
- Perform firm compressive vibrations to the chest wall during expiration (meet effigy 2). Movement sets up course vibrations in the airways to help loosen the secretions sticking to the walls of the airways.
- Vibrations should be avoided over patients breasts, spine and sternum to avert discomfort
- 1-5 minutes of vibration is usually performed in each selected position.
Figure 2: Mitt position for chest vibrations
Manual hyperinflation:
Manual hyperinflation should just be undertaken by nursing staff in the intensive care if it has been deemed an appropriate treatment past review from physiotherapy. Physiotherapists should provide nursing staff with documented plan for manual hyperinflation including maximum pressures and frequency of treatment.
Special Considerations
Should an aerosol generating process be undertaken on a patient under droplet precautions and so increment to airborne precautions by donning N95/P2 mask for at least the duration of the procedure.
Evidence Table
Bear witness table for this guideline can be found here.
References
-
Chaboyer, W., Gass, E., & Foster, One thousand. (2004). Patterns of chest physiotherapy in Australian Intensive Care Units. Journal of Critical Intendance, nineteen(three), 145-151. doi: http://dx.doi.org/10.1016/j.jcrc.2004.07.00
- Clini, E., & Ambrosino, North. (2005). Early physiotherapy in the respiratory intensive care unit. Respiritory Medicine, 99(9), 1096-1104. doi: x.1016/j.rmed.2005.02.02
- Denehy, L. (1999). The apply of manual hyperinflation in airway clearance. European Respiratory Journal, 14(four), 958-965. doi:10.1034/j.1399-3003.1999.14d38.x
- Fitzgerald, D. A., Follett, J., & Van Asperen, P. P. (2008;2009;). Assessing and managing lung disease and sleep disordered animate in children with cognitive palsy. Paediatric Respiratory Reviews, 10(1), xviii-24. doi:10.1016/j.prrv.2008.10.003
- Pountney, T. (2007). Neonatal Care Physiotherapy for Children (pp. 73-xc). Philadelphia: Elsevier Health Sciences.
- Harris, K., Clark, J., Coote, N., Fletcher, P., Harnden, A., McKean, Chiliad.. On behalf of the British Thoracic Guild Standards of Care Commission. (2011). British thoracic social club guidelines for the management of customs acquired pneumonia in children: Update 2011. Thorax, 66 Suppl 2(Suppl two), ii1-ii23. doi:x.1136/thoraxjnl-2011-200598
- Roqué i Figuls, M., Giné-Garriga, M., Granados Rugeles, C., Perrotta, C., & Vilaró, J. (2016). Breast physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database of Systematic Reviews(2). doi: 10.1002/14651858.CD004873.pub5
- Chatwin, M., Toussaint, K., Gonçalves, M. R., Sheers, N., Mellies, U., Gonzales-Bermejo, J., . . . Morrow, B. M. (2018). Airway clearance techniques in neuromuscular disorders: A state of the art review. Respiratory Medicine, 136, 98-110. doi:10.1016/j.rmed.2018.01.012
- Shann, F. (2014). Drug Doses (16th ed.): Intensive Intendance Unit, Royal Children's Hospital, Parkville, Commonwealth of australia.
- Tamburro, R. F., & Kneyber, M. C. (2015). Pulmonary specific ancillary treatment for pediatric acute respiratory distress syndrome: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatric Critical Intendance Medicine, 16(5 Suppl 1), S61-72. doi: 10.1097/pcc.0000000000000434
- Unsworth, A., Curtis, Yard., & Asha, S. E. (2015). Treatments for blunt chest trauma and their bear upon on patient outcomes and health service delivery. Scandinavian Journal of Trauma Resuscitation Emerg Medicine, 23, 17. doi: 10.1186/s13049-015-0091-5
Please remember to read the disclaimer.
The development of this nursing guideline was coordinated past Kate Lambert, CNC, Rosella Ward, Lisa Robson, Physiotherapist and approved past the Nursing Clinical Effectiveness Committee. Updated Nov 2020.
Source: https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Nurses_role_in_advanced_secretion_clearance/
0 Response to "Nursing Interventions You Need to Know to Promote Adequate Respiratory Function"
Post a Comment